|
Home |
Program |
Speakers |
Meeting Registration |
Hotel Reservation |
Hotel Information |
Fellow Presentations
Past Syposia |
RWCS 2011 Videos |
Exhibitor Information |
CME | ADA |
Submissions |
Contact
History and Presentation
CC: Rash
HPI:
- 50 y.o. M with hx of bipolar disorder, schizophrenia, asthma, cocaine abuse originally presents to the ER on 5/29/10 c/o L elbow swelling x several weeks with new drainage, as well as ecchymotic lesions on his ears that "occurred after using cocaine."
- P.E. from ER also notes erythematous papules on his extremities. Pt seen in ER by Orthopedics and is diagnosed with olecrenon bursitis. 15 cc serosanguinous fluid drained from bursa and Fluid is sent for culture x 2 (negative). Pt sent home with course of Augmentin. Per ER notes, pt educated on "risks of cocaine and instructed to stop taking drugs," also told to f/u with PMD, dermatology, and orthopedics. No toxicology screen is sent.
- On 6/3/10 the patient re-presents to ER c/o of worsening of his skin lesions. Further history is obtained and the patient states he first notice "dark spots" on his ears 6-8 months ago that resolved. One week prior to presentation he developed lesions on his ears, then on his lower extremities. The lesions were painful, changed from pink to purple to black, and also formed hemorrhagic bullae. He denies any recent cocaine use when originally questioned on this admission.
- Pt also c/o intermittent SOB and chest discomfort x 2 mos. Found to be in rapid Afib with RVR to 150s. He is treated with IV cardizem and spontaneously converts to NSR. Pt placed on heparin drip and admitted to medicine service. Dermatology and Rheumatology consulted the following day
PMHx: Bipolar disorder, schizophrenia, mild asthma
PSHx: none
Meds (outpt): Augmentin 875/125 mg bid, Beclomethasone inhaler 80 mcg BID, Abilify and Depakote (pt can't recall doses and states he hasn't taken these meds x 3 wks)
Allergies: NKDA
Social Hx: only drug use pt admits to is cocaine use 20 yrs ago (intranasal) denies other drug use, tobacco or ETOH, no recent travel, works as a waiter
Fam Hx: mother died of MI @ age 55, no fam hx of autoimmune diseases
ROS: neg for f/c's, n/v/d, Raynauds's dry mouth or eyes, malar rash, photosensitivity, oral or genital ulcers, cough, hemoptysis, hematuria, nose bleeds, recent infection
Physical Exam
VITALS: BP 105/70, P 90 (150s on arrival to ER), T98.2, R18, SaO2 97% RA
GEN: well-appearing NAD
HEENT: NC/AT, EOMI, PERRLA, no oral ulcers or malar rash, no LAD, helix and lobes of ears with violaceous to black, tender lesions BL with ulcers on lobes
CV: RRR, S1/S2, no m/r/g's
LUNG: CTA BL
ABDOM: + BS, soft, NT/ND, no HSM
EXT: 2+ DP pulses BL, no edema, no splinter hemorrhages or digital ulcers
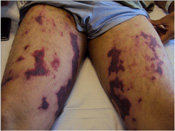
SKIN: large, 5-10 cm non-blanching violaceous to dusky plaques on LE's in a retiform pattern (sparing of palms and soles)
MSK: resolving L olecrenon bursitis, otherwise no swollen or tender joints
Labs/Studies
| Na |
139 |
| K |
4.5 |
| Cl |
103 |
| CO2 |
24 |
| BUN |
18 |
| Cr |
1.0 |
| Gluc |
102 |
| WBC |
3.3 72% gran |
| Hgb |
13.6 |
| Hct |
40.9 |
| Plt |
207 |
| Alb |
3.0 |
| TP |
5.9 |
| Bilitotal |
0.4 |
| Bilidirect |
0.1 |
| Alk Ø |
81 |
| ALT |
19 |
| AST |
14 |
UA: no blood, no protein
BCx neg x 4, UCx neg
ESR: 33
ANA: 1:40, dsDNA 77.0
Ro, La, Sm, RNP neg
C3 81, C4 13
RF 20, cryos neg
Hep C Ab, HepBsAg/HepBcAb neg; HIV neg
MPO ANCA 2.7 and PR3 ANCA 4.0 by ELISA
-ANCA by IF not done due to positive ANA
Anti-phospholipid panel: + Lupus Anti-Coagulant
Utox: + for opiates (cocaine neg)
TTE: normal EF, no vegetations, CXR: WNL
Hospital Course
- Pt was seen by dermatology and skin punch biopsy taken. Also seen by Rheumatology consult who recommend multiple serologies, an echo, and start pt on prednisone 60 mg daily. His lesions continue to expand including new lesions on cheeks. Pt now admits to using cocaine. C and p ANCA are positive, however, no evidence of internal organ involvement and findings could be consistnt with drug-induced vasculitis
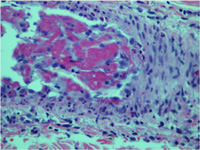
- Skin biopsy returns as vasculitis with thrombosis and necrosis – though non-specific these findings similar findings have been reported with cocaine-induced vasculopathy
- After discussion with derm and reviewing literature, pt's presentation was c/w cocaine/levamisole pseudovasculitis:
- Distrubution of lesions (ears/face)
- Biopsy results
- Leukopenia
- Positive serologies (ANCA/LAC/ANA)
- Pt developed worsening psychiatric symptoms (anxiety, hallucinations) on prednisone.
- Since there is no clear evidence of benefit of steroids in this self-limited, drug-induced condition, they were discontinued.
- Skin lesions remain stable and ear lesion improved
- Pt is d/c'd on hospital day # 10.
- Pt re-admitted with extensive cellulitis/superifection of the lesions on his LE's (reported improper wound care), required surgical debridement x 2.
- Pt lost to follow-up, serologies have not been repeated
Discussion
- Cocaine is widely used in the US - 2.1 million use cocaine per month according to National Survey on Drug use and Health (2007)
- Rheumatic manifestations due to cocaine have been described in literature1:
- ANCA positive syndromes mimicking Wegener's, MPA, Churg-Strauss
- HSP
- SSc/CREST/Raynauds
- Bullous skin lesions/Steven Johnson syndrome
- Cutaneous pseudovasculitis
- Cocaine-induced midline destructive lesions (CIMDL)
- Proposed mechanisms to explain vascular/autoimmune complications of cocaine include2:
- Vasconstrictive properties
- Activation of endothelial cells by cocaethylene, cocaine metabolite
- Cocaine-induced production of autoantibodies
- Cocaine-Induced Pseudovasculitis refers to pathologic findings of fibrin thrombi, hemorrhage and leukocytoclasis within the blood vessel. It is usually localized to the skin (reticular pattern) but can also have internal organ involvement. An inconsistent ANCA pattern is a diagnostic clue. Abstinence from cocaine is required to achieve resolution. Treatment is supportive, steroids have also been used although their effectiveness is controversial.3
- Recently, there have been multiple case reports of pseudovasculitis thought tobe secondary to cocaine contaminated with Levamisole:
- Walsh N et al. Cocaine-related retiform pupura: evidence to incriminate the adulterant, levamisole J Cutan Path. 2010. (2 pts)
- Buchanan JA et al. Levamisole-Induced Occlusive Necrotizing Vasculitis of the ears after use of cocaine contaminated with levamisole. J Med Toxicol Published online June 12 2010. (1 pt)
- Bradford M et al. Bilateral Necrosis of the Earlobes and Cheeks: Another complication of cocaine contaminated with Levamisole. Ann Int Med. 2010 Jun 1;152(11):758-9 (2 pts)
- Waller JM et al. Cocaine-associated retiform purpura and neutropenia: is levamisole the culprit? J Am Acad Dermatol (2010) 63(3) 530-535 (2 pts)
- Levamisole:
- originally developed as an anti-helminth agent and was previously used to treat various cancers and autoimmune disorders
- Common veterinary pharmaceutical and can be readily purchased2
- Widely used to "cut" cocaine
- In 2009, 70% of cocaine seized at US borders contained levamisole4
- Associated with autoantibody production: ANA, LAC, ANCA
- Enhances T cell activation and proliferation and increases neutrophil mobility and adherence5
- Purpuric skin lesions with a predilection for the ears have been previously reported with levamisole use5-6. Recent reports of cocaine-induce pseudovasculitis also describe this and was also seen in this case.
- Diagnostic clues for cocaine/levamisole induced pseudovasculitis:
- Leukopenia/bone marrow suppression
- Positive ANA, ANCA, ACL or LAC
- Characteristic pathology: leukocytoclastic and thrombotic vasculitis or purely vaso-occlusive
- Levamisole can be tested in serum and urine, but should be done within 48 hrs due to its short half-life
References
- Bhinder S, Majithia V. Cocaine use and its rheumatologic manifestations. Clin Rheumatol. 2007; 26:1192-1194.
- Walsh N et al. Cocaine-related retiform pupura- evidence to incriminate the adulterant, levamisole J Cutan Path. 2010. doi:10.111/j.1600-0560.2010.01613x
- Friedman DR, Wolfsthal SD. Cocaine-Induced Pseudovasculitis. Mayo Clin Proc. May 2005; 80(5):671-673
- CDC - Agranulocytosis associated with cocaine use. MMWR 58:1381-5
- Rongioletti F et al. Purpura of the ears: a distinctive vasculopathy with circulating complicating long-term treatment with levamisole in children. Br J Dermatol. 140: 948-951
- Menni S et al. Ear lobe bilateral necrosis by levamisole-induced occlusive vasculitis in a pediatric patient. Pediatr Dermatol. 1997 Nov-Dec;14(6):477-9.
|