|
|
|
Home |
Program |
Speakers |
Meeting Registration |
Hotel Reservation |
Hotel Information |
Fellow Presentations
Systemic Sclerosis Presenting with Malignant Pleural Effusion in a 33-year-old MaleVaani Jegapragasan, MD
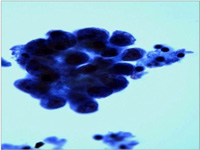
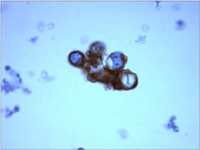
BackgroundMalignancy is associated with systemic sclerosis, both the limited and diffuse forms, in 3.6 to 10.7% . The diagnosis of systemic sclerosis may occur before, concurrent with, or after the diagnosis of malignancy. The average duration of follow-up from the development of systemic sclerosis to the development of lung cancer, however, is typically in the range of 5 to 9 years. Risk factors for the development of malignancy in patients with systemic sclerosis are female gender, increased age, and diffuse systemic sclerosis. Case DescriptionHPI 33 y/o male non-smoker with no significant PMH presented with progressive DOE over the past 1 month worsening over the past week associated with 7/10 left-sided pleuritic chest pain that awoke him from sleep, and a one-week history of night sweats prior to admission. He denied fever, weight loss, cough, hemoptysis, orthopnea, PND or lower ext swelling. No recent travel, sick contacts or known exposures to TB. He also denied occupational or environmental exposures. ROS positive for GERD symptoms and bluish discoloration of fingers and toes exacerbated by the cold consistent with Raynaud's phenomenon. Physical exam notable for decreased breath sounds over left lung field with dullness to percussion, tenderness to palpation over left ribs anteriorly at lower costal margin, cyanosis of distal fingertips, and waxy appearance of all fingers to level of MCP jointsHD#1: CXR showed a moderate to large left sided pleural effusion. Thoracentesis showed exudative fluid with lymphocytic predominance. HD#3: U/S-guided chest tube placement. CT chest showed 1.6 x 1.4 x 1.6 cm mass in LUL suspicious for a primary bronchogenic carcinoma. CT brain/abd/pelvis were unremarkable. HD#14, pt received first cycle of chemotherapy with taxol, carboplatin, and bevazicumab. Pleural Fluid Studies
Labs/Studies
Diagnosis
DiscussionEpidemiologyLung cancer is the most frequent type of cancer seen in patients with systemic sclerosis. The relative risk of lung cancer in patients with systemic sclerosis has been reported as high as 16.5 times that of normal patients. In a literature review by Yang et al, there was a significant non-smoker predominance in patients with systemic sclerosis and lung cancer compared with other connective tissue diseases. This review also found a significant predominance of bronchoalveolar cell carcinoma in patients with systemic sclerosis which has been reported to be 50-77%. This variety usually accounts for 4% of all lung cancers. PathophysiologyA variety of mechanisms have been postulated in systemic sclerosis patients that predispose them to malignancy:
Yang et al found that patients with pulmonary fibrosis appear prone to developing pulmonary malignancies. It has been suggested that diffuse interstitial fibrosis may cause atypical epithelial regenerative changes leading to neoplastic proliferation. One possible mechanism is through the effects of cytokines such as transforming growth factor-b which may cause excess cellular division resulting in transformation. Changes in the extracellular matrix, which play an important part in growth and differentiation, may also affect the behavior of normal cells. ConclusionThe pt was diagnosed with Stage IIIB non-small cell lung cancer which has a 5-year survival of ~5%. Given the advanced stage, the treatment is palliative and involves systemic chemotherapy. Increased vigilance for symptoms of cancer is recommended in patients with systemic sclerosis given the increased risk for malignancy in this population. Associations of malignancy with autoantibodies are the subject of some controversy. A study of 23 patients indicated a close temporal relationship between the onset of cancer and scleroderma in patients with antibodies to RNA polymerase I/III which is distinct from scleroderma patients with other autoantibody specificities (Shah 2010). References
|
|
Administrative Office: Contact: Home |
Program |
Speakers | Meeting Registration |
Hotel Reservation | Hotel Information |
Fellow Presentations
|